COVID19 Vaccine Information
Commonwealth of VA COVID19 Vaccination Plan
Introduction
In March 2020, the Commonwealth of Virginia established a Unified Command System to manage the state-level response to COVID-19. A Vaccine Unit was formed under the Public Health Surveillance and Guidance Workgroup of the Commonwealth’s unified command structure in June 2020 to conduct planning and coordination. Additionally, a COVID-19 Vaccine Advisory Workgroup was established in August 2020 to gather key stakeholder input on vaccine plans, priority groups, vaccine equity and other related issues. Virginia’s interim draft COVID-19 vaccination plan was developed by the Virginia Department of Health (VDH) and was recently exercised with partner state agencies. This plan will continue to be updated in collaboration with local health districts, the Virginia Emergency Support Team (VEST) and the COVID-19 Vaccine Advisory Workgroup as the federal government shares additional details and more information becomes available about the vaccine(s). The most current information, including the full version of Virginia’s interim draft COVID-19 Vaccination Plan, is available.
Vaccine Information for Consumers
It’s important for everyone to continue using all the tools available to help stop this pandemic as we learn more about how COVID-19 vaccines work in real-world conditions. Cover your mouth and nose with a mask when around others, stay at least 6 feet away from others, avoid crowds, and wash your hands often.

Because COVID-19 is a new disease with new vaccines, you may have questions about what happens before, during, and after your appointment to get vaccinated. These tips will help you know what to expect when you get vaccinated, what information your provider will give you, and resources you can use to monitor your health after you are vaccinated.
Before Vaccination
- See if COVID-19 vaccination is recommended for you right now.
- Learn more about the different types of COVID-19 vaccines and how they work.
- Learn more about the benefits of getting a COVID-19 vaccination.
- When you go to your appointment, remember to cover your mouth and nose with a mask when you are around others and stay at least 6 feet away from others. Learn more about protecting yourself from COVID-19 during visits to the doctor or a pharmacy.
When You Get Vaccinated
- You should receive a vaccination card or printout that tells you what COVID-19 vaccine you received, the date you received it, and where you received it.
- You should receive a paper or electronic version of a fact sheet that tells you more about the specific COVID-19 vaccine you are being offered. Each authorized COVID-19 vaccine has its own fact sheet that contains information to help you understand the risks and benefits of receiving that specific vaccine.

After Vaccination
- With most COVID-19 vaccines, you will need two shots in order for them to work. Get the second shot even if you have side effects after the first one, unless a vaccination provider or your doctor tells you not to get a second shot.
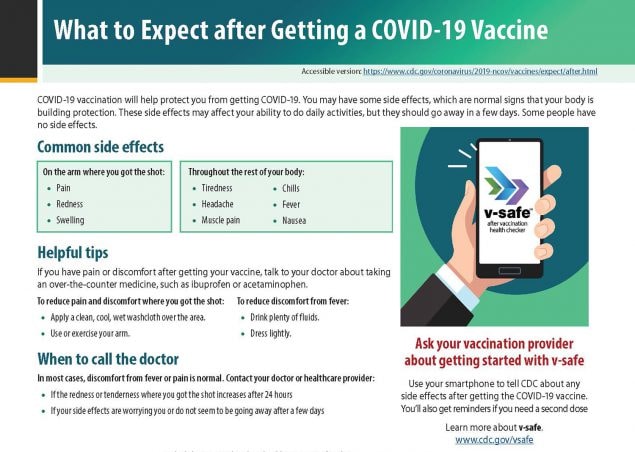
- Ask your healthcare provider about getting started with v-safe, a free, smartphone-based tool that uses text messaging and web surveys to provide personalized health check-ins after you receive a COVID-19 vaccination. V-safe also reminds you to get your second dose if you need one. Learn more at www.cdc.gov/vsafe.
- It takes time for your body to build protection after any vaccination. COVID-19 vaccines that require 2 shots may not protect you until a week or two after your second shot.
Learn about common side effects and get helpful tips on how to reduce your pain and discomfort.
COVID-19 vaccination will help protect you from getting COVID-19. You may have some side effects, which are normal signs that your body is building protection. These side effects may affect your ability to do daily activities, but they should go away in a few days.
Common side effects
On the arm where you got the shot:
- Pain
- Swelling
Throughout the rest of your body:
- Fever
- Chills
- Tiredness
- Headache
Helpful tips
If you have pain or discomfort, talk to your doctor about taking an over-the-counter medicine, such as ibuprofen or acetaminophen.
To reduce pain and discomfort where you got the shot:
- Apply a clean, cool, wet washcloth over the area.
- Use or exercise your arm.
To reduce discomfort from fever:
- Drink plenty of fluids.
- Dress lightly.
When to call the doctor
In most cases, discomfort from fever or pain is normal. Contact your doctor or healthcare provider:
- If the redness or tenderness where you got the shot increases after 24 hours
- If your side effects are worrying you or do not seem to be going away after a few days
Remember
- Side effects may feel like flu and even affect your ability to do daily activities, but they should go away in a few days.
- With most COVID-19 vaccines, you will need 2 shots in order for them to work. Get the second shot even if you have side effects after the first shot, unless a vaccination provider or your doctor tells you not to get a second shot.
- It takes time for your body to build protection after any vaccination. COVID-19 vaccines that require 2 shots may not protect you until a week or two after your second shot.
It’s important for everyone to continue using all the tools available to help stop this pandemic as we learn more about how COVID-19 vaccines work in real-world conditions. Cover your mouth and nose with a mask when around others, stay at least 6 feet away from others, avoid crowds, and wash your hands often.
PDF Fact Sheet for Healthcare Providers to Give after Vaccination
Infection prevention and control considerations for healthcare personnel with systemic signs and symptoms following COVID-19 vaccination
Note: Strategies are needed for healthcare facilities to appropriately evaluate and manage post-vaccination signs and symptoms among healthcare personnel (HCP). The approach described in this document is intended to reduce the risks for disruptions in care and pathogen (e.g., SARS-CoV-2) transmission resulting from:
- unnecessarily excluding HCP with only post-vaccination signs and symptoms from work, and
- inadvertently allowing HCP with SARS-CoV-2 or another transmissible infection to work.
These considerations are based on the current understanding of signs and symptoms following COVID-19 vaccination, including timing and duration, and might change as experience with the vaccine accumulates.
Overview
Systemic signs and symptoms, such as fever, fatigue, headache, chills, myalgia, and arthralgia, can occur following COVID-19 vaccination. Preliminary dataexternal icon from mRNA COVID-19 vaccine trials indicate that most systemic post-vaccination signs and symptoms are mild to moderate in severity, occur within the first three days of vaccination (the day of vaccination and following two days, with most occurring the day after vaccination), resolve within 1-2 days of onset, and are more frequent and severe following the second dose and among younger persons compared to those who are older (>55 years). Cough, shortness of breath, rhinorrhea, sore throat, or loss of taste or smell are not consistent with post-vaccination symptoms, and instead may be symptoms of SARS-CoV-2 or another infection.
Because systemic post-vaccination signs and symptoms might be challenging to distinguish from signs and symptoms of COVID-19 or other infectious diseases, HCP with postvaccination signs and symptoms could be mistakenly considered infectious and restricted from work unnecessarily; this might have negative consequences for HCP, patients, and long-term care facility residents. Hence, strategies are needed to effectively manage post-vaccination systemic signs and symptoms and limit unnecessary work restrictions.
The strategies in this document are intended for use by occupational health programs and public health officials and apply to all HCP working in healthcare settings. Because information is currently lacking on vaccine effectiveness in the general population; the resultant reduction in disease, severity, or transmission; or the duration of protection, vaccinated HCP should continue to follow all current infection prevention and control recommendations to protect themselves and others from SARS-CoV-2 infection.
Considerations to minimize the impact of post-vaccination systemic signs and symptoms on healthcare staffing include:
- Vaccinating HCP preceding 1-2 days off, during which they are not required to be in the facility.
- Staggering delivery of vaccine to HCP in the facility so that not all HCP in a single department, service, or unit are vaccinated at the same time. Staggering considerations may be more important following the second dose when systemic symptoms after vaccination, such as fever, are more likely to occur.
- Informing HCP about the potential for short-term systemic signs and symptoms post-vaccination and potential options for mitigating them if symptoms arise (e.g., nonsteroidal anti-inflammatory medications or acetaminophen).
- Developing a strategy to provide timely assessment of HCP with systemic signs and symptoms post-vaccination, including providing or identifying options for SARS-CoV-2 viral testing, so it is readily available if indicated. Testing should have rapid turnaround time from collection time to result reporting (< 24 to 48 hours).
- Offering nonpunitive sick leave options (e.g., paid sick leave) for HCP with systemic signs and symptoms post-vaccination to remove barriers to reporting these symptoms.
Suggested approaches to evaluating and managing new-onset systemic post-vaccination signs and symptoms in HCP
The approaches described below apply to HCP who have received COVID-19 vaccination in the prior 3 days (including day of vaccination, which is considered day 1) and are not known to have had unprotected exposure to SARS-CoV-2 in a community or healthcare setting in the previous 14 days. Symptomatic HCP who are within 14 days of an unprotected exposure to SARS-CoV-2 in a community or a higher risk exposure in a healthcare setting should be excluded from work and evaluated for SARS-CoV-2 infection.
The approaches suggested in the table below should be tailored to fit the clinical and epidemiologic characteristics of each specific case. Ultimately, clinical judgement should be used to determine the likelihood of infection versus post-vaccination symptoms and the indicated clinical approach.
Positive viral (nucleic acid or antigen) tests for SARS-CoV-2, if performed, should not be attributed to the COVID-19 vaccine, as vaccination does not influence the results of these tests.
Note: The following signs and symptoms, alone, are not consistent with SARS-CoV-2 infection and should be managed per usual protocols for vaccine-related side effects:
- immediate hypersensitivity reactions (e.g., urticaria, anaphylaxis)
- local symptoms (e.g., pain, swelling, or redness at injection site)
| HCP Signs and Symptoms | Suggested approach | Additional notes |
|---|---|---|
| Signs and symptoms unlikelyto be from COVID-19 vaccination:Presence of ANYsystemic signs and symptoms consistent with SARS-CoV-2 infection (e.g., cough, shortness of breath, rhinorrhea, sore throat, loss of taste or smell) or another infectious etiology (e.g., influenza) that are not typical for post-vaccination signs and symptoms. | Exclude from work pending evaluation for possible etiologies, including SARS-CoV-2 infection, as appropriate.Criteria for return to work depends on the suspected or confirmed diagnosis. Information on return to work for HCP with SARS-CoV-2 infection is available here. | If performed, a negative SARS-CoV-2 antigen test in HCP who have signs and symptoms that are not typical for post-vaccination signs and symptoms should be confirmed by SARS-CoV-2 nucleic acid amplification test (NAAT). Further information on testing is available here:https://www.cdc.gov/coronavirus/2019-nCoV/lab/index.html |
| Signs and symptoms that maybe from either COVID-19 vaccination, SARS-CoV-2 infection, or another infection:Presence of ANYsystemic signs and symptoms (e.g., fever, fatigue, headache, chills, myalgia, arthralgia) that are consistent with post-vaccination signs and symptoms, SARS-CoV-2 infection or another infectious etiology (e.g., influenza).
Fever in healthcare settings is defined as a measured temperature of 100.0oF (37.8oC) or higher. |
Evaluate the HCP.HCP who meet the following criteria may be considered for return to work without viral testing for SARS-CoV-2:
Feel well enough and are willing to work and Are afebrile* and Systemic signs and symptoms are limited only to those observed following COVID-19 vaccination (i.e., do not have other signs and symptoms of COVID-19 including cough, shortness of breath, sore throat, or change in smell or taste). If symptomatic HCP return to work, they should be advised to contact occupational health services (or another designated individual) if symptoms are not improving or persist for more than 2 days. Pending further evaluation, they should be excluded from work and viral testing should be considered. If feasible, viral testing could be considered for symptomatic HCP earlier to increase confidence in the cause of their symptoms. *HCP with fever should, ideally, be excluded from work pending further evaluation, including consideration for SARS-CoV-2 testing. If an infectious etiology is not suspected or confirmed as the source of their fever, they may return to work when they feel well enough. In facilities where critical staffing shortages are anticipated or occurring, HCP with fever and systemic signs and symptoms limited only to those observed following vaccination could be considered for work if they feel well enough and are willing. These HCP should be re-evaluated, and viral testing for SARS-CoV-2 considered, if fever does not resolve within 2 days. |
If performed, a negative SARS-CoV-2 antigen test in HCP who have symptoms that are limited only to those observed following COVID-19 vaccination (i.e., do not have cough, shortness of breath, sore throat, or change in smell or taste) may not require confirmatory SARS-CoV-2 NAAT testing. Additional information is available here: https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antigen-tests-guidelines.html |
Note: Additional guidance to mitigate staff shortages when work restrictions are recommended but there are no longer enough staff to provide safe patient care is available in Strategies to Mitigate Healthcare Personnel Staffing Shortages.
Additional Resources:
Infection prevention and control considerations for residents of long-term care facilities with systemic signs and symptoms following COVID-19 vaccination can be found at:
https://www.cdc.gov/coronavirus/2019-ncov/hcp/post-vaccine-considerations-residents.html
Further information on COVID-19 vaccines and recommendations can be found at:
https://www.cdc.gov/vaccines/covid-19/index.html
https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19.html
Adverse events that occur in a recipient following COVID-19 vaccination should be reported to VAERS. Vaccination providers are required by the Food and Drug Administration to report vaccination administration errors, serious adverse events, cases of Multisystem Inflammatory Syndrome, and cases of COVID-19 that result in hospitalization or death following COVID-19 vaccination under Emergency Use Authorization. Reporting is encouraged for any other clinically significant adverse event even if it is uncertain whether the vaccine caused the event. Information on how to submit a report to VAERS is available at https://vaers.hhs.govexternal icon or by calling 1-800-822-7967.
Definitions:
Healthcare Personnel (HCP): HCP refers to all paid and unpaid persons serving in healthcare settings who have the potential for direct or indirect exposure to patients or infectious materials, including body substances (e.g., blood, tissue, and specific body fluids); contaminated medical supplies, devices, and equipment; contaminated environmental surfaces; or contaminated air. HCP include, but are not limited to, emergency medical service personnel, nurses, nursing assistants, home healthcare personnel, physicians, technicians, therapists, phlebotomists, pharmacists, students and trainees, contractual staff not employed by the healthcare facility, and persons not directly involved in patient care, but who could be exposed to infectious agents that can be transmitted in the healthcare setting (e.g., clerical, dietary, environmental services, laundry, security, engineering and facilities management, administrative, billing, and volunteer personnel).
Healthcare settings refers to places where healthcare is delivered and includes, but is not limited to, acute care facilities, long-term acute care facilities, inpatient rehabilitation facilities, nursing homes and assisted living facilities, home healthcare, vehicles where healthcare is delivered (e.g., mobile clinics), and outpatient facilities, such as dialysis centers, physician offices, and others.
Serious adverse event: Serious adverse events are defined as death; a life-threatening adverse event; inpatient hospitalization or prolongation of existing hospitalization; a persistent or significant incapacity or substantial disruption of the ability to conduct normal life functions; a congenital anomaly/birth defect; an important medical event that based on appropriate medical judgement may jeopardize the individual and may require medical or surgical intervention to prevent one of the outcomes listed in this definition.
Infection prevention and control considerations for residents of long-term care facilities with systemic signs and symptoms following COVID-19 vaccination
Note: Strategies are needed by long-term care facilities to appropriately evaluate and manage post-vaccination signs and symptoms among their residents. The approach described in this document is intended to balance:
- the risk of unnecessary testing and implementation of Transmission-Based Precautions for residents with only post-vaccination signs and symptoms with that of
- inadvertently allowing residents with infectious COVID-19 or another transmissible infectious disease to expose others in the facility.
While this guidance is intended for long-term care facilities, it could also be applied to patients in other healthcare settings. These considerations are based on the current understanding of signs and symptoms following COVID-19 vaccination, including timing and duration, and might change as experience with the vaccine accumulates.
Overview
Systemic signs and symptoms, such as fever, fatigue, headache, chills, myalgia, and arthralgia, can occur following COVID-19 vaccination. Preliminary dataexternal icon from mRNA COVID-19 vaccine trials indicate that most systemic post-vaccination signs and symptoms are mild to moderate in severity, occur within the first three days of vaccination (the day of vaccination and following two days, with most occurring the day after vaccination), resolve within 1-2 days of onset, and are more frequent and severe following the second dose and among younger persons compared to those who are older (>55 years). Cough, shortness of breath, rhinorrhea, sore throat, or loss of taste or smell are not consistent with post-vaccination symptoms, and instead may be symptoms of SARS-CoV-2 or another infection.
Note: The following signs and symptoms, alone, are not consistent with SARS-CoV-2 infection and should be managed per usual protocols for vaccine-related side effects:
- immediate hypersensitivity reactions (e.g., urticaria, anaphylaxis)
- local symptoms (e.g., pain, swelling, or redness at injection site)
Routine infection prevention and control practices:
Healthcare personnel at long-term care facilities should follow the recommended infection prevention and control practices described in the Preparing for COVID-19 in Nursing Homes and the Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic. These recommendations, which emphasize close monitoring of residents of long-term care facilities for symptoms of COVID-19, universal source control, physical distancing (when possible), hand hygiene, and optimizing engineering controls, are intended to protect healthcare personnel and residents from exposures to SARS-CoV-2. Use of personal protective equipment (PPE), including universal use of a facemask and eye protection for healthcare personnel in areas experiencing moderate to substantial community transmission who are caring for residents not suspected to have SARS-CoV-2 infection, is also recommended.
Because information is currently lacking on vaccine effectiveness in the general population; the resultant reduction in disease, severity, or transmission; or the duration of protection, residents and healthcare personnel should continue to follow all current infection prevention and control recommendations to protect themselves and others from SARS-CoV-2 infection, regardless of their vaccination status.
Suggested approaches to evaluating and managing systemic new onset post-vaccination signs and symptoms for residents in long-term care facilities.
The approaches described in the Table below apply to residents who have received COVID-19 vaccination in the prior 3 days (including day of vaccination, which is considered day 1).
Note: Facilities that are conducting outbreak testing for SARS-CoV-2 transmission, or evaluating residents who have had prolonged close contact with someone with SARS-CoV-2 infection in the previous 14 days, should care for residents following all recommended infection control practicesincluding placement in Transmission-Based Precautions with use of all recommended personal protective equipment, and performing appropriate testing.
All symptomatic residents should be assessed; the approaches suggested in the table below should be tailored to fit the clinical and epidemiologic characteristics of the specific case.
In any situation, positive viral (nucleic acid or antigen) tests for SARS-CoV-2, if performed, should not be attributed to the COVID-19 vaccine, as vaccination does not influence the results of these tests.
| Signs and Symptoms | Suggested approach | Additional notes |
|---|---|---|
| Signs and symptoms unlikely to be from COVID-19 vaccination:Presence of ANY systemic signs and symptoms consistent with SARS-CoV-2 (e.g., cough, shortness of breath, rhinorrhea, sore throat, loss of taste or smell) or another infectious etiology (e.g., influenza) that are not typical for post-vaccination signs and symptoms | Evaluate for possible infectious etiologies, including testing for SARS-CoV-2 and/or other pathogens, as appropriate.Pending evaluation, these residents should be placed in a single person room (if available) and cared for by healthcare personnel wearing all PPE recommended for residents with suspected or confirmed SARS-CoV-2 infection. They should not be cohorted with residents with confirmed SARS-CoV-2 infection unless they are also confirmed to have SARS-CoV-2 infection through testing.
Criteria for when Transmission-Based Precautions may be discontinued depend on the results of the evaluation. |
If performed, a negative SARS-CoV-2 antigen test in a resident who has signs and symptoms that are not typical for post-vaccination signs and symptoms should be confirmed by SARS-CoV-2 nucleic acid amplification test (NAAT). Further information on testing is available here: https://www.cdc.gov/coronavirus/2019-nCoV/lab/index.html |
| Signs and symptoms that may befrom either COVID-19 vaccination, SARS-CoV-2 infection, or another infection:Presence ofANY systemic signs and symptoms (e.g., fever, fatigue, headache, chills, myalgia, arthralgia) that are consistent with post-vaccination signs and symptoms, SARS-CoV-2 infection, or another infectious etiology (e.g., influenza). Fever in long-term care settings is defined as a single measured temperature of 100.0oF (37.8oC) or higher or repeated temperatures of 99.0oF (37.2oC). |
Evaluate the resident.These residents should be restricted to their current room (except for medically necessary procedures) and closely monitored until:
Healthcare personnel caring for these residents should, ideally, wear all PPE recommended for residents with suspected or confirmed SARS-CoV-2 infection while evaluating the cause of these symptoms. Strategies to optimize PPE supply are available here: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/index.html If the resident’s symptoms resolve within 2 days, precautions can be discontinued. Fever, if present, should have resolved for at least 24 hours before discontinuing precautions. Viral testing for SARS-CoV-2 should be considered for residents if their symptoms are not improving or persist for longer than 2 days. |
If SARS-CoV-2 antigen testing is used to evaluate a symptomatic resident, a negative antigen test in a resident who has symptoms that are limited only to those observed following COVID-19 vaccination (i.e., do not have cough, shortness of breath, rhinorrhea, sore throat, or loss of taste or smell) may not require confirmatory SARS-CoV-2 NAAT.However, confirmatory SARS-CoV-2 NAAT testing should be conducted if there is active transmission in the facility, if the resident has had prolonged close contact with someone with SARS-CoV-2 infection in the prior 14 days, or if symptoms persist for longer than 2 days.
Additional information is available here: https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antigen-tests-guidelines.html |
Additional Resources:
Infection prevention and control considerations for healthcare personnel with systemic signs and symptoms following COVID-19 vaccination can be found at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/post-vaccine-considerations-healthcare-personnel.html
Additional information on COVID-19 vaccines and recommendations:
https://www.cdc.gov/vaccines/covid-19/index.html
https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19.html
Adverse events that occur in a recipient following COVID-19 vaccination should be reported to VAERS. Vaccination providers are required by the Food and Drug Administration to report vaccination administration errors, serious adverse events, cases of Multisystem Inflammatory Syndrome, and cases of COVID-19 that result in hospitalization or death following COVID-19 vaccination under Emergency Use Authorization. Reporting is encouraged for any other clinically significant adverse event even if it is uncertain whether the vaccine caused the event. Information on how to submit a report to VAERS is available at https://vaers.hhs.govexternal icon or by calling 1-800-822-7967.
Definitions:
Serious adverse event: Serious adverse events are defined as death; a life-threatening adverse event; inpatient hospitalization or prolongation of existing hospitalization; a persistent or significant incapacity or substantial disruption of the ability to conduct normal life functions; a congenital anomaly/birth defect; an important medical event that based on appropriate medical judgement may jeopardize the individual and may require medical or surgical intervention to prevent one of the outcomes listed in this definition.
Pfizer-BioNTech Vaccine Information

General Information:
Diluent: 0.9% sodium chloride (normal saline, preservative-free)
Mix before using
Multi-dose vial: 5 doses per vial Dosage: 0.3 mL
Age Indications:
16 years of age and older
Schedule:
2 doses series separated by 21 days
Both doses must be COVID-19 vaccine (Pfizer)
Administer:
Intramuscular (IM) injection in the deltoid muscle
Pfizer-BioNTech COVID-19 Vaccine Webpage
Moderna Vaccine Information
Moderna COVID-19 Vaccine Webpage
Vaccine Storage Safety
 Loading…
Loading…
